Phimosis vs. Paraphimosis: A Comprehensive Guide
Table of Contents
- 1 Phimosis vs. Paraphimosis: A Comprehensive Guide
- 1.1 Introduction
- 1.2 Phimosis: Unveiling the Tight Foreskin Challenge
- 1.3 Phimosis vs. Paraphimosis: A Comparative Analysis
- 1.4 Causes of Phimosis
- 1.5 Symptoms and Signs
- 1.6 Complications of Untreated Phimosis
- 1.7 Paraphimosis: The Perils of Retracted Foreskin
- 1.8 Unveiling Paraphimosis
- 1.9 Causes Leading to Paraphimosis
- 1.10 Recognizing Symptoms
- 1.11 Complications of Neglected Paraphimosis
- 1.12 Phimosis vs. Paraphimosis: A Comparative Analysis
- 1.13 Recognizing and Managing Phimosis and Paraphimosis Symptoms in Children
- 1.14 Exploring Treatment Options and Proactive Measures
- 1.15 Treatment Approaches for Phimosis
- 1.16 Addressing Paraphimosis: Swift and Decisive Measures
- 1.17 Additional Considerations and Lifestyle Impacts
- 1.18 Conclusion: Navigating Male Genital Health with Confidence
- 2 FAQs: Answering Common Queries
- 3 Conclusion
In this article we discover the difference between Phimosis vs. Paraphimosis in this comprehensive guide. Get insights, expert advice, and answers to FAQs on these conditions. Read on for a detailed understanding about phimosis vs. paraphimosis by Dr. k.k. pandey.
Introduction
Navigating the intricacies of male genital health involves understanding terms like phimosis and paraphimosis. This article aims to shed light on the distinctions, causes, symptoms, and potential complications associated with these conditions. Whether you’re seeking information for yourself or a loved one, this guide provides valuable insights.
Phimosis: Unveiling the Tight Foreskin Challenge
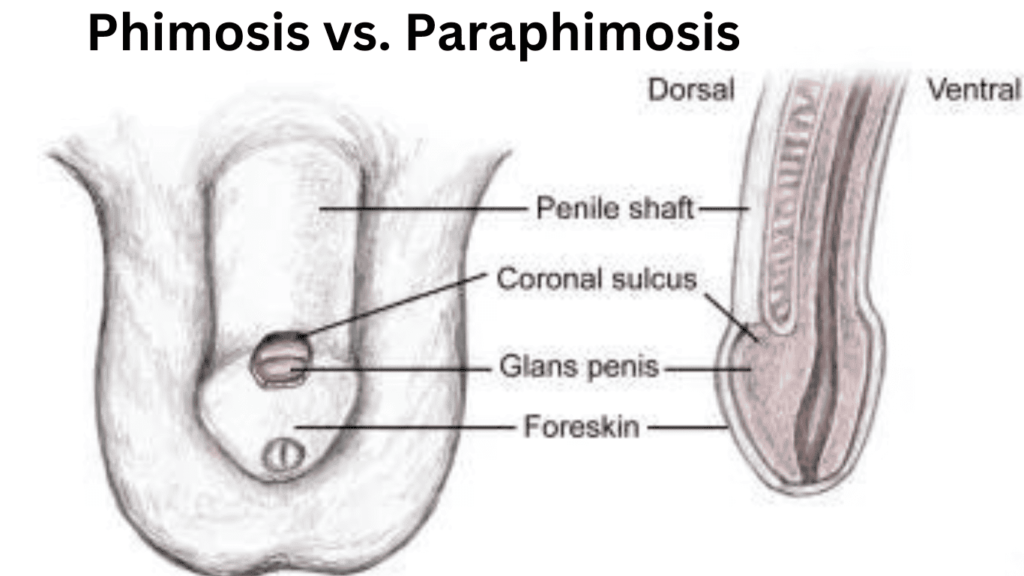
Phimosis vs. Paraphimosis: A Comparative Analysis
Causes of Phimosis
Unraveling the origins of phimosis, we explore congenital factors and acquired causes such as infections or inflammation. Delving into these roots is crucial for understanding the condition’s nature.
Symptoms and Signs
Identifying phimosis involves recognizing symptoms like difficulty retracting the foreskin, pain during urination, and potential inflammation or infection. Awareness of these signs is essential for early intervention.
Complications of Untreated Phimosis
Neglecting phimosis can lead to severe complications, including recurrent infections, painful erections, and challenges in maintaining proper genital hygiene. Addressing the condition promptly is crucial to prevent long-term issues.
Paraphimosis: The Perils of Retracted Foreskin
Unveiling Paraphimosis
Paraphimosis emerges when the foreskin, once retracted, cannot return to its original position. This can lead to constriction of blood vessels, causing swelling and potential complications. Understanding the mechanics is pivotal for grasping the severity of the situation.
Causes Leading to Paraphimosis
Forceful retraction of the foreskin is a common cause of paraphimosis. This section explores scenarios that may trigger this condition, emphasizing the importance of gentle care in this sensitive area.
Recognizing Symptoms
Identifying paraphimosis involves recognizing symptoms such as swelling, pain, and potential discoloration of the glans due to reduced blood flow. Early detection is crucial for effective management.
Complications of Neglected Paraphimosis
Left untreated, paraphimosis can escalate, causing tissue damage, necrosis, and necessitating surgical intervention in severe cases. Acknowledging the potential complications underscores the urgency of seeking medical attention.
Phimosis vs. Paraphimosis: A Comparative Analysis
In this section, we draw a side-by-side comparison of phimosis and paraphimosis, highlighting their distinct features, causes, symptoms, and potential consequences. Understanding these differences is pivotal for accurate diagnosis and tailored treatment.
Recognizing and Managing Phimosis and Paraphimosis Symptoms in Children
Phimosis and paraphimosis are conditions that may affect young boys, and it’s important for parents to be aware of the symptoms to ensure prompt medical attention if needed. While each child’s experience may vary, here are common signs associated with these conditions:
Symptoms of Phimosis:
- Bulging of the Foreskin: Some children may exhibit bulging of the foreskin, particularly during urination.
- Delayed Foreskin Retraction: Inability to fully retract the foreskin by the age of 3, though the timeline for this process may vary among individuals.
Symptoms of Paraphimosis:
- Swelling of the Penis Tip: Noticeable swelling at the tip of the penis when attempting to pull back the foreskin.
- Pain: Children may experience pain, both when attempting to retract the foreskin and during urination.
- Inability to Pull Foreskin Back: The foreskin cannot be pulled back over the tip of the penis, causing discomfort.
- Discoloration of the Penis Tip: The tip of the penis may appear dark red or blue in color, indicating potential circulation issues.
- Painful Urination: Discomfort or pain during urination can be an additional symptom of paraphimosis.
- Decreased Urinary Stream: Parents may notice a reduced urinary stream in affected children.
Seeking Medical Attention:
It’s crucial to note that the symptoms of phimosis vs. paraphimosis can be mistaken for other health conditions. If parents observe any of these signs in their child, consulting a healthcare provider is essential for an accurate diagnosis.
Emergency Situation – Paraphimosis:
Paraphimosis is considered a medical emergency. If parents suspect their child is experiencing paraphimosis, seeking, immediate medical care is imperative to prevent complications.
Understanding the symptoms associated with phimosis and paraphimosis in children is crucial for early detection and appropriate medical intervention. Parents should be vigilant and seek professional advice if any concerns arise, with particular urgency in cases of suspected paraphimosis. Early identification and management can contribute to the well-being and healthy development of the child.
Exploring Treatment Options and Proactive Measures
Treatment Approaches for Phimosis
Circumcision: A Definitive Solution
Circumcision remains the primary treatment for pathologic phimosis, especially in children. This surgical procedure involves the removal of the foreskin, addressing the underlying issue and preventing future complications. It’s crucial to note that circumcision is not only a solution but also a preventive measure against potential recurrence.
Preputioplasty: Preserving the Foreskin
For those seeking an alternative to circumcision, preputioplasty is an option. This surgical approach focuses on preserving the foreskin while addressing the tightness issue. Postoperative care involves regular foreskin retraction, gradually allowing the attainment of a normal retractile prepuce.
Topical Treatments: A Non-Surgical Avenue
In certain cases, a prospective study suggests the efficacy of 0.1% mometasone furoate in treating severe phimosis. While this offers a non-surgical option, individual responses may vary, and consultation with a healthcare professional is essential.
Addressing Paraphimosis: Swift and Decisive Measures
Immediate Medical Attention is Paramount
Paraphimosis demands immediate medical intervention due to its potential complications. If identified, seeking prompt help can prevent further vascular compromise, reducing the risk of severe outcomes.
Circumcision as a Preventive Measure
While circumcision is often associated with treating phimosis, it also serves as a preventive measure against paraphimosis. By removing the foreskin, the risk of entrapment and subsequent complications diminishes significantly.
Additional Considerations and Lifestyle Impacts
Hygiene Practices: A Crucial Component
Maintaining good genital hygiene is a cornerstone in preventing both phimosis and paraphimosis. Regular cleaning, particularly in uncircumcised individuals, can significantly reduce the risk of scarring and related complications.
Age-Related Risks: Understanding the Dynamics
Elderly individuals may face an increased risk of phimosis due to the loss of skin elasticity and infrequent erections. Recognizing age-related factors is vital for proactive management.
Educational Outreach for Prevention
Educational initiatives should emphasize the importance of gentle care, proper hygiene, and the potential risks associated with forceful retraction. Outreach to both individuals and caregivers can contribute to early identification and intervention.
In conclusion, understanding the nuances of phimosis and paraphimosis empowers individuals to make informed decisions about their health. From recognizing symptoms to exploring treatment options, this comprehensive guide aims to provide clarity and support.
Seeking professional medical advice for accurate diagnosis and personalized guidance is crucial for anyone experiencing symptoms related to phimosis or paraphimosis. Remember, proactive measures, timely interventions, and a commitment to good genital hygiene contribute to maintaining male genital health with confidence.
Phimosis vs. Paraphimosis–https://youtu.be/CX0AHKqhxa8
FAQs: Answering Common Queries
Q: Can phimosis or paraphimosis resolve on its own?
A: While some cases may improve with age, it’s advisable to seek medical attention for a proper diagnosis and personalized guidance.
Q: Are there non-surgical treatments for phimosis or paraphimosis?
A: Yes, homeopathic medicines, topical steroids, stretching exercises, and proper hygiene may be recommended. However, consult a healthcare professional for individualized advice.
Q: How common are phimosis and paraphimosis?
A: Both conditions are relatively common, with varying prevalence across different age groups.
Q: Can phimosis or paraphimosis cause long-term complications?
A: Yes, if left untreated, both conditions can lead to serious complications, emphasizing the importance of early intervention.
Q: Is paraphimosis a medical emergency?
A: Yes, it requires immediate medical attention to prevent potential complications.
Q: Can lifestyle changes help prevent phimosis or paraphimosis?
A: Maintaining good genital hygiene and avoiding forceful retraction can contribute to prevention. However, individual factors play a role.
Conclusion
Navigating the nuances of phimosis vs. paraphimosis is essential for promoting male genital health. This comprehensive guide has provided insights into the causes, symptoms, and complications associated with these conditions. If you suspect any issues, seeking prompt medical advice ensures timely intervention and optimal outcomes.