“Unearthing Hidden Gems: 10 Intriguing Facts About the Champions League”
Can tic syndrome be cured? This is the main question inthe mind of every parents which child is suffering from Tourette syndrome.
What is Tic Syndrome?
Table of Contents
- 1 What is Tic Syndrome?
- 2 Prevalence and Impact on Daily Life
- 3 Symptoms of tic syndrome
- 4
- 5 Why It’s Essential to Explore Various Treatment Options for Tic Syndrome
- 6 Causes of Tic Syndrome
- 7 Diagnosis of Tic Syndrome
- 8 Can Tic Syndrome Be Cured?
- 9 Treatment Options for Tic Syndrome
- 10 Emerging Treatments and Research for Tic Syndrome
- 11 Living with Tic Syndrome
- 12 Myths and Misconceptions
- 13 Conclusion
- 14 FAQs
Definition and Types
Tic Syndrome refers to a group of neurodevelopmental disorders characterized by involuntary, repetitive movements and vocalizations called tics. These can range from mild to severe and can significantly impact daily functioning. It is a attention deficit hyperactivity disorder (adhd).
1. Transient Tic Disorder
Definition: A condition where tics occur for a short duration, typically less than a year is called as Transient Tic Disorder.
Symptoms: Simple motor tics like eye blinking or facial grimacing, and vocal tics such as throat clearing or grunting.
Prognosis: Often resolves on its own without the need for treatment.
2. Chronic Tic Disorder
Definition: Tics that persist for more than one year.
Symptoms: Can include both motor and vocal tics, though not necessarily both. Examples include head jerking or repeated sniffing.
Prognosis: Symptoms may fluctuate in severity and can persist into adulthood, although some individuals may experience a reduction in symptoms over time.
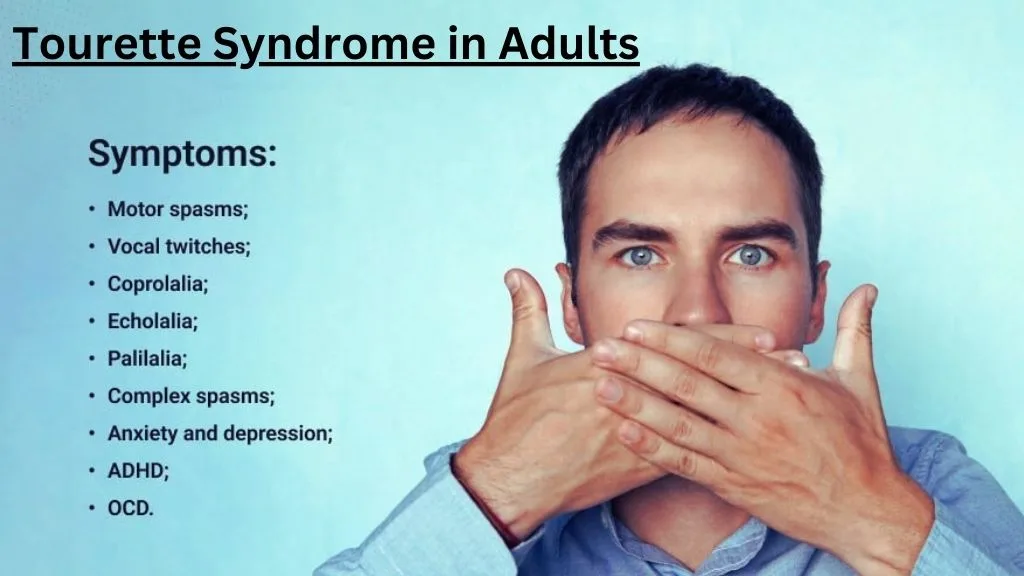
3. Tourette Syndrome
Definition: A more complex tic disorder involving multiple motor tics and at least one vocal tic that have been present for more than one year.
Symptoms: Includes complex tics such as jumping, spinning, or uttering words or phrases. It often coexists with other conditions like ADHD and OCD.
Prognosis: Tics can vary in intensity and may change over time. While some individuals experience a decrease in tics during late adolescence or adulthood, others may continue to have symptoms throughout their lives.
Prevalence and Impact on Daily Life
Prevalence:
– Tic disorders are relatively common in childhood. Transient tic disorder affects an estimated 5-25% of school-aged children.
– Chronic tic disorder affects about 1-2% of the population.
– Tourette syndrome is less common, affecting approximately 0.3-0.8% of children and adolescents.
Impact on Daily Life:
Social and Emotional Impact: Individuals with tic disorders may experience social stigma, bullying, and isolation due to their symptoms. This can result in diminished self-worth, heightened anxiety, and increased depression.
Academic and Occupational Challenges: Tics can interfere with concentration and learning in school, as well as productivity in the workplace. Frequent tics can be distracting and may require accommodations.
Physical Discomfort and Injury: Repeated tics can cause physical pain or injury, such as headaches from head jerking or muscle strain from repetitive movements.
Quality of Life: The presence of tics can affect overall quality of life, making everyday activities more challenging and stressful.
Symptoms of tic syndrome
Tic syndrome encompasses a range of disorders characterized by involuntary, repetitive movements and sounds. The symptoms can vary widely in terms of type, frequency, and severity. Here’s a detailed overview of the symptoms associated with tic syndrome:
1. Motor Tics
Motor tics are involuntary movements that can be simple or complex.
- Simple Motor Tics: These involve brief, repetitive movements of a single muscle group. Examples include:
– Eye blinking
– Facial grimacing
– Shoulder shrugging
– Head jerking
2. Complex Motor Tics**: These involve coordinated movements that may appear purposeful. Examples include:
– Touching objects or people
– Jumping
– Twirling
– Mimicking others’ actions (echopraxia)
2. Vocal (Phonic) Tics
Vocal tics are involuntary sounds generated by the movement of air through the nose, mouth, or throat.
- Simple Vocal Tics: These are brief and often meaningless sounds. Examples include:
– Throat clearing
– Sniffing
– Grunting
– Coughing
2. Complex Vocal Tics: These are more meaningful and may include words or phrases. Examples include:
– Repeating one’s own words or phrases (palilalia)
– Repeating others’ words or phrases (echolalia)
– Using obscene or socially inappropriate language (coprolalia)
3. Onset and Course
– Onset: Tic disorders typically begin in childhood, with the average onset between ages 5 and 7.
– Course: The severity and frequency of tics can vary over time. Tics often peak in severity during early adolescence and may decrease or change in adulthood.
4. Associated Conditions
Tic disorders are often associated with other conditions, which can influence the presentation and management of symptoms.
– Attention-Deficit/Hyperactivity Disorder (ADHD): Many individuals with tic disorders also have ADHD, characterized by hyperactivity, impulsiveness, and difficulty sustaining attention.
– Obsessive-Compulsive Disorder (OCD): OCD is common in individuals with tic disorders and involves repetitive, intrusive thoughts (obsessions) and ritualistic behaviors (compulsions).
– Anxiety and Depression: Anxiety disorders and depression are also more prevalent among those with tic disorders.
5. Triggers and Aggravating Factors
Several factors can exacerbate tic symptoms.
Stress and Anxiety: High levels of stress and anxiety can increase the frequency and severity of tics.
Excitement or Fatigue: Being overly excited or tired can also trigger tics.
Environmental Factors: Changes in routine, major life events, and certain environmental factors can influence tic severity.
6. Diagnosis
Diagnosing tic disorders involves a comprehensive evaluation by a healthcare professional, including a detailed medical history and clinical observation of symptoms. There are no specific tests for tic disorders, but diagnostic criteria from the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) are used.
Why It’s Essential to Explore Various Treatment Options for Tic Syndrome
1. Individual Variability in Symptoms
– Diverse Presentations: Tic disorders, including Transient Tic Disorder, Chronic Tic Disorder, and Tourette Syndrome, manifest differently in each individual. The types, frequency, and severity of tics vary widely, necessitating personalized treatment approaches.
– Tailored Interventions: What works for one person may not work for another. Exploring a range of treatment options allows for the customization of care to best meet the unique needs of each individual.
2. Managing Comorbid Conditions
– Associated Disorders: Many individuals with tic disorders also have co-occurring conditions such as ADHD, OCD, anxiety, or depression. Comprehensive treatment plans that address both tics and comorbid conditions are essential for overall well-being.
– Holistic Approach: A variety of treatment options can help manage not just tics but also the symptoms of associated conditions, leading to more effective and holistic care.
3. Enhancing Quality of Life
– Daily Functioning: Tics can interfere with daily activities, social interactions, academic performance, and occupational productivity. Effective treatment can reduce the impact of tics on these areas.
– Social and Emotional Well-Being: Reducing the frequency and severity of tics can improve self-esteem, reduce anxiety, and enhance social interactions, leading to a better quality of life.
4. Long-Term Management
– Chronic Nature of Tic Disorders: While some tic disorders, like Transient Tic Disorder, may resolve on their own, others like Chronic Tic Disorder and Tourette Syndrome often require long-term management. A variety of treatment options ensures sustained effectiveness over time.
– Adaptability: As individuals grow and their symptoms change, having multiple treatment options allows for adjustments in their care plan, ensuring continued effectiveness and adaptability.
5. Minimizing Side Effects
– Medication Side Effects: Some pharmacological treatments can cause significant side effects. Exploring non-pharmacological options, such as behavioral therapies or homeopathic treatments, can provide symptom relief with fewer adverse effects.
– Balanced Approach: A combination of treatments can be used to minimize the reliance on medications, thereby reducing the risk of side effects while still effectively managing symptoms.
6. Advancements in Research
– Emerging Therapies: Ongoing research continually introduces new treatment options. Staying informed about the latest advancements allows individuals to benefit from cutting-edge therapies.
– Innovative Approaches: Exploring various treatment options ensures that individuals are not limited to traditional methods but can also consider innovative and potentially more effective treatments.
7. Empowering Individuals and Families
– Informed Decision-Making: Knowledge of multiple treatment options empowers individuals and families to make informed decisions about their care.
– Active Participation: Exploring various treatments encourages active participation in managing the disorder, fostering a sense of control and agency over the condition.
Causes of Tic Syndrome
1. Genetic Factors
– Hereditary Influence: Research indicates that tic disorders often run in families, suggesting a genetic component. If a parent or sibling has a tic disorder, the likelihood of developing tics increases.
– Specific Genes: Although the exact genes involved are not fully understood, studies have identified several genetic markers that may contribute to the risk of developing tic disorders.
2. Environmental Influences
– **Prenatal and Perinatal Factors**: Various environmental factors during pregnancy and childbirth may increase the risk of tic disorders. These include:
– **Maternal Stress**aSZWZQ: High levels of stress during pregnancy can affect fetal brain development.
– **Prenatal Exposure**: Exposure to tobacco, alcohol, or illicit drugs during pregnancy has been linked to a higher incidence of tic disorders.
– **Complications at Birth**: Premature birth, low birth weight, and birth complications such as hypoxia can increase the risk of tic disorders.
– **Postnatal Environment**: Early childhood experiences, including trauma, infections, and exposure to environmental toxins, may also contribute to the development of tics.
3. Neurological Basis
– **Brain Structure and Function**: Abnormalities in certain brain regions, particularly the basal ganglia, are associated with tic disorders. The basal ganglia are involved in the control of movement and motor functions.
– **Neurotransmitter Imbalance**: Dysregulation of neurotransmitters, particularly dopamine, is believed to play a crucial role in tic disorders. Dopamine pathways in the brain are involved in regulating movement, and abnormalities in these pathways can lead to tics.
– **Neural Circuitry**: Disruptions in the neural circuits connecting the basal ganglia, thalamus, and cortex may contribute to the onset and persistence of tics.
4. Associated Conditions
– Attention-Deficit/Hyperactivity Disorder (ADHD): A significant number of individuals with tic disorders also have ADHD. The coexistence of these conditions suggests shared neurobiological mechanisms.
– Obsessive-Compulsive Disorder (OCD): Tic disorders frequently co-occur with OCD, indicating a potential overlap in the underlying neural pathways and genetic factors.
– Anxiety and Mood Disorders: High levels of anxiety and depression are common among individuals with tic disorders, which can exacerbate tic severity and complicate treatment.
5. Immune System Dysfunction
– PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections): This is a subset of tic disorders triggered by streptococcal infections. The immune response to the infection may mistakenly target brain tissues, leading to the sudden onset or worsening of tics and OCD symptoms.
– Autoimmune Mechanisms: Emerging research suggests that other autoimmune processes may also be involved in the development of tic disorders, though this area requires further investigation.
Diagnosis of Tic Syndrome
Diagnosing tic syndrome involves a comprehensive approach that includes clinical evaluation, medical history, and sometimes additional tests to rule out other conditions. The procedure generally includes these steps:
1. Clinical Evaluation
– Observation of Tics: A healthcare provider, usually a neurologist or psychiatrist, will observe the frequency, type, and severity of tics. This includes noting both motor tics (e.g., blinking, grimacing) and vocal tics (e.g., grunting, throat clearing).
– Duration of Symptoms: To diagnose tic disorders, it is essential to establish the duration of tics. For transient tic disorder, tics must be present for at least one month but less than a year. For chronic tic disorder and Tourette syndrome, tics must persist for more than a year.
2. Medical History
– Comprehensive History: A detailed medical history is crucial. This includes a history of the tics (when they started, how they have changed over time) and any associated symptoms or conditions, such as ADHD or OCD.
– Family History: Since tic disorders can be hereditary, a family history of tics or related conditions is important. This can provide insights into the genetic component of the disorder.
– Developmental History: Information about the individual’s developmental milestones, any prenatal or perinatal complications, and early childhood illnesses or exposures can help in understanding potential contributing factors.
3. Diagnostic Criteria
– **DSM-5 Criteria**: The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides specific criteria for diagnosing tic disorders:
– **Tourette Syndrome**: Requires the presence of both multiple motor tics and one or more vocal tics, persisting for more than a year, with onset before age 18.
– **Chronic Tic Disorder**: Requires either motor tics or vocal tics (but not both) that persist for more than a year, with onset before age 18.
– **Provisional (Transient) Tic Disorder**: Involves motor and/or vocal tics that have been present for at least one month but less than a year, with onset before age 18.
4. Neurological Examination
– **Physical Examination**: A thorough neurological examination is performed to rule out other neurological disorders that could cause similar symptoms. This includes assessing motor function, coordination, and reflexes.
– **Rule Out Other Conditions**: Conditions such as dystonia, chorea, and myoclonus can mimic tics, so it is important to differentiate between these and true tic disorders.
5. Additional Tests
– **Neuroimaging**: Although not typically required for diagnosis, brain imaging (such as MRI or CT scans) may be conducted if there are atypical symptoms or if the diagnosis is unclear. This helps rule out structural brain abnormalities.
– **Laboratory Tests**: Blood tests or other laboratory work may be done to rule out metabolic or infectious causes of tics, such as thyroid dysfunction or streptococcal infection in cases of suspected PANDAS.
6. Psychological Assessment
– **Behavioral and Cognitive Evaluation**: Assessments may be performed to evaluate for coexisting conditions like ADHD, OCD, anxiety, or depression. These evaluations help in developing a comprehensive treatment plan.
– **Impact on Daily Life**: Understanding how tics affect the individual’s daily functioning, including school or work performance, social interactions, and emotional well-being, is crucial for diagnosis and management.
Can Tic Syndrome Be Cured?
The question of whether tic syndrome can be cured is complex and depends on various factors including the type of tic disorder, the individual’s age, and the presence of co-occurring conditions. Below is an in-depth examination of this subject:
1. Current Scientific Understanding
– **Nature of Tic Disorders**: Tic disorders, including Transient Tic Disorder, Chronic Tic Disorder, and Tourette Syndrome, are typically chronic conditions that manifest in childhood. While some children may outgrow their tics, others may continue to experience them into adulthood.
– **No Universal Cure**: As of now, there is no universal cure for tic disorders. However, many individuals experience a significant reduction in symptoms over time, particularly during late adolescence or early adulthood.
2. Differences Between Managing and Curing
– **Symptom Management**: Most treatment approaches focus on managing and reducing the severity and frequency of tics rather than curing the disorder. Effective management can lead to a substantial improvement in quality of life.
– **Potential for Remission**: Some individuals, particularly those with transient tic disorder, may see their tics disappear entirely without treatment. In chronic cases, while complete remission is rare, long periods of reduced symptoms are possible.
3. Long-Term Prognosis
– **Transient Tic Disorder**: Many children with transient tic disorder outgrow their tics within a year without the need for treatment.
– **Chronic Tic Disorder and Tourette Syndrome**: These conditions often persist for longer periods, but the severity of tics usually diminishes with age. Many adults with Tourette Syndrome report fewer and less severe tics.
– **Individual Variation**: The long-term prognosis varies widely among individuals. Some may experience significant improvement, while others may continue to have tics into adulthood.
4. Factors Influencing Outcomes
– **Early Intervention**: Early diagnosis and intervention can help manage symptoms more effectively, potentially leading to better long-term outcomes.
– **Co-occurring Conditions**: The presence of co-occurring conditions like ADHD or OCD can complicate the prognosis and may require comprehensive treatment strategies.
– **Lifestyle and Support**: A supportive environment, stress management techniques, and healthy lifestyle choices can positively impact the management of tic disorders.
5. Emerging Treatments and Research
– **Advancements in Research**: Ongoing research is exploring new treatment options, including genetic therapies, neuromodulation techniques, and advanced behavioral therapies. These emerging treatments hold promise for more effective management and potentially better outcomes in the future.
– **Clinical Trials**: Participation in clinical trials can provide access to cutting-edge treatments and contribute to the broader understanding of tic disorders.
Treatment Options for Tic Syndrome
Managing tic syndrome involves a variety of approaches tailored to the individual’s specific needs and the severity of their symptoms. The primary goal of treatment is to reduce the frequency and intensity of tics and improve the individual’s quality of life. Here are the main treatment options:
1. Behavioral Therapies
Behavioral therapies are often the first line of treatment for tic disorders, especially for mild to moderate cases.
a. Cognitive Behavioral Therapy (CBT)
– Overview: CBT helps individuals recognize and change problematic thoughts and behaviours associated with their tics.
– Effectiveness: Particularly useful for managing co-occurring conditions like OCD and anxiety that can exacerbate tics.
b. Habit Reversal Training (HRT)
– Overview: HRT teaches individuals to become more aware of their tics and trains them to perform a competing response when they feel the urge to tic.
– Techniques: Awareness training, relaxation techniques, and development of competing responses (e.g., gently clenching a fist instead of head jerking).
c. Comprehensive Behavioral Intervention for Tics (CBIT)
– Overview: CBIT combines HRT with other behavioral strategies to manage tics.
– Components: Includes habit reversal, relaxation techniques, and functional intervention strategies to reduce tic-related impairments.
2. Medications
Medications may be prescribed when tics are severe and significantly impact daily functioning.
a. Antipsychotics
– **Common Drugs**: Haloperidol, pimozide, and risperidone.
– **Effectiveness**: Can reduce the severity of tics, but may have side effects like weight gain, sedation, and movement disorders.
b. ADHD Medications
– **Common Drugs**: Methylphenidate and clonidine.
– **Effectiveness**: Useful for individuals with co-occurring ADHD; some medications can reduce tics, while others may exacerbate them.
c. Other Medications
– **Alpha-2 Adrenergic Agonists**: Clonidine and guanfacine can help reduce tics and are also used for managing ADHD symptoms.
– **Anticonvulsants**: Topiramate may be beneficial for some individuals.
3. Homeopathic Treatments
Homeopathy was an alternative treatment approach that some individuals choose to explore before but now a days, it is the main line of treatment for the SLE.
Overview of Homeopathy
Principles: Homeopathy is based on the idea of treating “like with like” and using highly diluted substances to stimulate the body’s self-healing processes.
Commonly Used Remedies:
1- Hyoscyamus niger: Used for treating nervous tics and twitching.
2- Zincum metallicum: Often prescribed for individuals with restless movements and jerking.
3- Agaricus muscarius: Used for involuntary movements and spasms.
Evidence and Research on Effectiveness
– Studies: There is much scientific evidence supports the efficacy of homeopathy for tic disorders. Most evidence is practical on the patients and proof by removing the symptoms of the disease.
– Considerations: Important to consult with homeopathic professional for starting any homeopathic treatment. Don’t do self-medication because it can be dangerous to the patient.
– Potential Risks: There is no risk to take medication with a qualified and experienced homeopathic practitioner.
– **Interactions**: No possible interactions with other medications.
– **Quality Control**: Ensuring remedies are sourced from reputable practitioners.
4. Lifestyle and Home Remedies
Non-medical interventions can also play a significant role in managing tic disorders.
a. Stress Management Techniques
– **Relaxation Exercises**: Deep breathing, progressive muscle relaxation, and yoga can help reduce stress, which may in turn reduce tic frequency.
– **Mindfulness and Meditation**: Techniques to increase awareness and control over body movements.
b. Diet and Nutrition
– **Healthy Diet**: Maintaining a balanced diet can support overall health and well-being.
– **Nutritional Supplements**: Omega-3 fatty acids, magnesium, and other supplements may be beneficial, although evidence is limited.
c. Physical Activity
– Regular Exercise: Can help reduce stress and improve overall physical and mental health.
– Types of Exercise: Activities such as swimming, cycling, and walking are beneficial and can be adjusted based on individual preferences and abilities.
5. Emerging Treatments and Research
New therapies and ongoing research continue to provide hope for more effective treatments in the future.
– **Recent Advancements**
– **Genetic Therapies**: Research into genetic causes of tic disorders may lead to targeted treatments.
– **Neuromodulation Techniques**: Methods such as deep brain stimulation (DBS) are being explored for severe cases.
– **Clinical Trials**
– **Participation**: Joining clinical trials can provide access to cutting-edge treatments and contribute to the broader understanding of tic disorders.
Emerging Treatments and Research for Tic Syndrome
Research into tic syndrome and related conditions is ongoing, leading to the development of innovative therapies and treatment approaches. Here are some emerging treatments and areas of research:
1. Genetic Therapies
– **Understanding Genetic Causes**: Advances in genetics have identified specific genes and genetic variations associated with tic disorders. Research aims to further elucidate the genetic basis of tic syndrome, potentially leading to targeted genetic therapies.
– **Gene Editing Techniques**: CRISPR-Cas9 and other gene editing technologies hold promise for correcting genetic mutations linked to tic disorders. These approaches could offer personalized treatments tailored to an individual’s genetic profile.
2. Neuromodulation Techniques
Deep Brain Stimulation (DBS): DBS involves implanting electrodes into specific brain regions to modulate neural activity. While still in the early stages of research, DBS shows potential for treating severe cases of tic disorders that do not respond to other therapies.
Transcranial Magnetic Stimulation (TMS): TMS is a non-invasive neuromodulation technique that uses magnetic fields to stimulate targeted brain areas. Studies have shown promising results in reducing tics, although further research is needed to optimize treatment protocols.
3. Pharmacological Innovations
Novel Medications: Pharmaceutical companies are developing new medications targeting neurotransmitter systems implicated in tic disorders. These medications aim to provide symptom relief with fewer side effects compared to traditional antipsychotics.
Precision Medicine Approaches: Advances in pharmacogenomics allow for personalized medication selection based on an individual’s genetic profile, optimizing treatment efficacy and minimizing adverse reactions.
4. Behavioral and Cognitive Therapies
Virtual Reality (VR) Therapy: VR technology is being integrated into behavioral therapy interventions for tic disorders. Virtual environments can simulate real-life situations, allowing individuals to practice coping strategies and habit reversal techniques in a controlled setting.
Telemedicine and Digital Health Platforms: Remote delivery of behavioral therapy interventions via telemedicine platforms and mobile apps offers convenient access to care, particularly for individuals in remote or underserved areas.
5. Complementary and Alternative Medicine
Mindfulness-Based Interventions: Mindfulness meditation and mindfulness-based stress reduction techniques show promise in reducing tic severity and improving overall well-being. Research is ongoing to further explore their efficacy as adjunctive treatments.
Nutritional Interventions: Studies are investigating the role of diet and nutritional supplements in managing tic disorders. Certain dietary modifications and supplements, such as omega-3 fatty acids and magnesium, may have beneficial effects on tic symptoms.
6. Translational Research
Bridging Basic Science and Clinical Practice: Translational research aims to translate findings from laboratory studies into clinical applications. By bridging the gap between basic science and clinical practice, translational research accelerates the development of novel treatments for tic disorders.
Patient-Centered Research: Engaging individuals with tic disorders and their families in research efforts ensures that treatments align with their needs and preferences. Patient-centered research focuses on improving outcomes and quality of life from the patient’s perspective.
7. Collaborative Initiatives
– **International Collaborations**: Collaborative initiatives bring together researchers, clinicians, advocacy groups, and individuals affected by tic disorders from around the world. These collaborations facilitate knowledge sharing, data pooling, and the development of standardized treatment guidelines.
– **Interdisciplinary Approaches**: Integrating insights from neuroscience, psychology, genetics, and other disciplines enhances our understanding of tic disorders and informs multidisciplinary treatment approaches.
Living with Tic Syndrome
Living with tic syndrome can present unique challenges, but with proper support, coping strategies, and management techniques, individuals can lead fulfilling lives. Here’s a comprehensive guide on living with tic syndrome:
1. Education and Awareness
– Understanding the Condition: Educate yourself and others about tic syndrome, including its symptoms, causes, and treatment options. Increased awareness reduces stigma and promotes acceptance and support within the community.
– Advocacy: Advocate for yourself or your loved one by sharing experiences, raising awareness, and advocating for improved access to healthcare and support services.
2. Building a Support Network
– **Family and Friends**: Surround yourself with understanding and supportive family members and friends who can offer emotional support and encouragement.
– **Support Groups**: Joining support groups or online communities for individuals with tic disorders can provide a sense of belonging, validation, and practical advice from others who share similar experiences.
– **Professional Support**: Seek guidance from healthcare professionals, including neurologists, psychiatrists, psychologists, and therapists specializing in tic disorders.
3. Developing Coping Strategies
– **Tic Awareness**: Learn to recognize triggers, sensations, and warning signs associated with tics. Increased awareness can help anticipate and manage tic episodes more effectively.
– **Stress Management**: Practice stress-reduction techniques such as deep breathing, meditation, yoga, or mindfulness to minimize stress levels, which can exacerbate tic symptoms.
– **Distraction Techniques**: Engage in activities that divert attention away from tics, such as hobbies, sports, music, or creative pursuits.
– **Acceptance and Self-Compassion**: Practice self-compassion and acceptance of tic symptoms as part of who you are. Treat yourself with kindness and understanding and celebrate your strengths and achievements.
4. Communicating Effectively
– **Open Communication**: Communicate openly and honestly with family members, friends, teachers, employers, and healthcare providers about your tic syndrome. Clarify misconceptions, share your needs, and discuss strategies for accommodating your symptoms.
– **Educating Others**: Educate those around you about tic disorders, including how they manifest and how they can best support you. Encourage empathy, patience, and non-judgmental attitudes.
5. Seeking Treatment and Support Services
– **Comprehensive Treatment Plan**: Work with healthcare providers to develop a personalized treatment plan that may include behavioral therapies, medications, and lifestyle modifications.
– **Regular Monitoring**: Stay in regular contact with healthcare providers to monitor tic symptoms, adjust treatment as needed, and address any concerns or complications.
– **Accessing Support Services**: Explore available support services such as occupational therapy, speech therapy, and social skills training to address specific challenges related to tic disorders.
6. Navigating Daily Life
– **Education and Employment**: Advocate for accommodations and support at school or work to facilitate academic and occupational success. This may include flexible schedules, breaks, or modified assignments.
– **Social Interactions**: Foster supportive relationships and social connections while navigating social situations. Educate peers about tic disorders and focus on shared interests and activities.
– **Self-Care**: Prioritize self-care practices, including adequate sleep, nutrition, exercise, and relaxation techniques, to support overall health and well-being.
7. Embracing Personal Growth
– Resilience and Adaptability: Embrace challenges as opportunities for growth and resilience-building. Focus on strengths, cultivate optimism, and adapt to changes with flexibility and creativity.
– Setting Realistic Goals: Set achievable goals and celebrate progress, no matter how small. Break tasks into manageable steps and recognize your efforts along the way.
– Finding Meaning and Purpose: Explore interests, passions, and aspirations that bring fulfilment and meaning to your life. Engage in activities that align with your values and contribute to your sense of purpose.
Living with tic syndrome requires patience, resilience, and self-compassion. By building a strong support network, developing effective coping strategies, seeking appropriate treatment and support services, and embracing personal growth, individuals with tic disorders can navigate life’s challenges and thrive in their journey towards well-being and fulfilment.
Myths and Misconceptions
Dispelling myths and misconceptions about tic syndrome is crucial for promoting understanding, empathy, and support for individuals affected by these conditions. Here are some prevalent myths along with the actual truths:
Myth: Tic disorders are just bad habits that individuals can control if they try hard enough.
Truth: Tic disorders, including Tourette Syndrome, are neurological conditions characterized by involuntary movements or vocalizations. While individuals may sometimes suppress their tics temporarily, this often leads to increased tension and discomfort, and tics typically resurge later.
Myth: All individuals with tic disorders curse or make socially inappropriate gestures.
Truth: While coprolalia (the involuntary utterance of obscene or socially inappropriate words or phrases) is a symptom of Tourette Syndrome, it affects only a minority of individuals with the condition. Most people with tic disorders have motor or vocal tics that are not socially inappropriate.
Myth: Tic disorders are caused by emotional trauma or poor parenting.
Truth: Tic disorders have a complex aetiology involving genetic, neurological, and environmental factors. While stress and anxiety can sometimes exacerbate tic symptoms, they do not cause tic disorders. Blaming parents or individuals for tic disorders perpetuates stigma and misunderstanding.
Myth: Tic disorders are rare and only affect children.
Truth: Tic disorders are more common than previously thought and can affect individuals of all ages. While symptoms often emerge during childhood, they can persist into adulthood. Additionally, many individuals with mild tic disorders may go undiagnosed or misdiagnosed.
Myth: Tics are always disruptive and impairing.
Truth: While tics can be disruptive and impairing for some individuals, others may have mild symptoms that do not significantly interfere with daily functioning. Tic severity varies widely among individuals, and many people with tic disorders lead fulfilling and successful lives.
Myth: Tic disorders are untreatable and cannot be managed effectively.
Truth: While there is no cure for tic disorders, various treatments and interventions can help manage symptoms and improve quality of life. Behavioral therapies, medications, lifestyle modifications, and support services can all play a role in effective management.
Myth: People with tic disorders are intellectually impaired or have other cognitive deficits.
Truth: Tic disorders do not affect intelligence or cognitive abilities. Many individuals with tic disorders have average or above-average intelligence and excel academically and professionally. It’s important to recognize that tic disorders are neurological conditions separate from cognitive functioning.
Myth: Individuals with tic disorders should just “snap out of it” or “ignore” their tics.
Truth: Tics are involuntary and not under conscious control. Telling someone to stop their tics is unhelpful and can increase stress and anxiety, which may exacerbate symptoms. Supportive and understanding responses are more beneficial.
Myth: Tic disorders are a sign of weakness or moral failing.
Truth: Tic disorders are medical conditions with a biological basis. They are not indicative of weakness, moral character, or personal failing. Stigmatizing attitudes toward tic disorders contribute to shame and discrimination and hinder access to appropriate care and support.
Myth: Tic disorders are contagious or can be transmitted through contact.
Truth: Tic disorders are not contagious and cannot be transmitted through contact or exposure. They are neurological conditions with genetic, environmental, and neurobiological factors contributing to their development.
Dispelling these myths and educating others about tic disorders promotes empathy, acceptance, and support for individuals affected by these conditions. By fostering understanding and reducing stigma, we can create a more inclusive and supportive environment for everyone.
Conclusion
In conclusion, tic syndrome, encompassing a spectrum of disorders such as transient tic disorder, chronic tic disorder, and Tourette syndrome, presents unique challenges for individuals and their families. Despite prevailing misconceptions, it’s essential to approach tic disorders with empathy, understanding, and accurate information.
Dispelling myths and misconceptions surrounding tic disorders is crucial for fostering acceptance and support within communities. Understanding that tic disorders are neurological conditions, not behavioral choices or signs of weakness, is fundamental to providing appropriate support and care.
Effective management of tic disorders involves a multifaceted approach, including behavioral therapies, medications, lifestyle modifications, and support services. By addressing symptoms comprehensively and tailoring treatment plans to individual needs, individuals with tic disorders can lead fulfilling lives.
Research into tic disorders continues to advance, offering hope for innovative therapies and improved outcomes. Genetic therapies, neuromodulation techniques, and emerging treatments underscore the ongoing commitment to enhancing the lives of those affected by tic disorders.
Ultimately, promoting awareness, acceptance, and access to resources is key to supporting individuals living with tic syndrome. By fostering a culture of understanding and compassion, we can create a more inclusive society where everyone feels valued and supported, regardless of their neurological differences.
FAQs
Q 1. What is tic syndrome?
Ans- Tic syndrome, or tic disorders, refers to a group of neurological conditions characterized by repetitive, involuntary movements (motor tics) and/or sounds (vocal tics). These tics can vary in frequency, intensity, and complexity.
Q 2. What are the types of tic disorders?
Ans- The main types of tic disorders include:
– Transient Tic Disorder: Tics are present for less than a year.
– Chronic Tic Disorder: Tics persist for more than a year.
– Tourette Syndrome: Multiple motor and vocal tics persist for more than a year, with onset before age 18.
Q 3. What causes tic disorders?
Ans- The exact cause of tic disorders is not fully understood, but it is believed to involve a combination of genetic, neurological, and environmental factors. Family history, abnormalities in brain structure or function, and imbalances in neurotransmitters may contribute to the development of tic disorders.
Q 4. Are tic disorders contagious?
Ans- No, tic disorders are not contagious. They are neurological conditions and cannot be transmitted through contact or exposure to individuals with tic disorders.
Q 5. Can tic disorders be cured?
Ans- While there is no cure for tic disorders, many individuals experience a reduction in symptoms over time, particularly with appropriate treatment and management strategies. Treatment focuses on minimizing the impact of tics on daily functioning and improving quality of life.
Q 6. Are all tics involuntary?
Ans- Yes, tics are involuntary movements or sounds that individuals cannot control voluntarily. Although some individuals may be able to suppress their tics temporarily, doing so often leads to increased discomfort and tension, and the tics typically resurge later.
Q 7. Do all individuals with tic disorders have coprolalia (involuntary swearing)?
Ans- No, coprolalia is a symptom of Tourette Syndrome but only affects a minority of individuals with the condition. Most people with tic disorders have motor or vocal tics that are not socially inappropriate.
Q 8. How are tic disorders treated?
Ans- Treatment for tic disorders may include behavioral therapies (such as habit reversal training), medications (such as antipsychotics or alpha-2 adrenergic agonists), lifestyle modifications, and support services. The choice of treatment depends on the individual’s symptoms and needs.
Q 9. Can tic disorders affect academic or occupational performance?
Ans- Yes, tic disorders can sometimes interfere with academic or occupational performance, particularly if tics are frequent or severe. However, with appropriate support and accommodations, many individuals with tic disorders are able to succeed academically and professionally.
Q 10. Where can I find support for tic disorders?
Ans- Support groups, online communities, advocacy organizations, and healthcare professionals specializing in tic disorders can provide valuable support, information, and resources for individuals and families affected by tic disorders.